Interpreting a knee joint X-ray is a critical skill for healthcare professionals. It provides valuable insights into the structure and potential issues within the knee. This article delves into the complexities of examining knee joint radiographs. It focuses on identifying normal results and understanding the implications of various radiographic parameters. By examining key angles, ratios, and grades, practitioners can accurately assess the condition of the knee joint. They can then make informed decisions regarding patient care.
Key Takeaways
- Strictly controlled conditions for anterior-posterior radiographs are essential to minimize bias from knee flexion angle or patient positioning.
- Radiographic parameters, such as the hip-knee-ankle angle, weight-bearing line ratio, and Kellgren-Lawrence grading system, are crucial for a comprehensive knee evaluation.
- Challenges in identifying articular surface landmarks and individual morphological variability can impact the precision of radiographic measurements.
- Statistical analysis reveals significant inter-observer reliability in assessing key radiographic parameters, underscoring their importance in clinical evaluations.
- Radiographic findings have direct clinical relevance, aiding in surgical planning, understanding knee function, and predicting disease progression.
Key Radiographic Parameters for Knee Joint X-Ray Evaluation
Understanding the Hip-Knee-Ankle Angle
The hip-knee-ankle angle plays a critical role in assessing the alignment of the lower limb. Healthcare professionals measure it on a full limb radiograph. This measurement reflects the overall angular relationship between the hip, knee, and ankle joints. In addition, a normal hip-knee-ankle angle is crucial for balanced weight distribution across the knee joint during standing and walking. A variation from the normal range can suggest misalignment, which may lead to joint pain and degenerative changes over time.
To accurately measure this angle, radiologists must identify specific landmarks on the hip, knee, and ankle. Then, observers calculate the angle by drawing lines through these landmarks and measuring the resulting angle formed at the knee. The following table summarizes the inter-observer reliability of the hip-knee-ankle angle measurement, thereby indicating its reproducibility among different observers:
| Group | ICC (Interclass Correlation Coefficient) | 95% Confidence Interval | p-value |
| A | 0.980 | 0.967–0.988 | < 0.001 |
| B | 0.967 | 0.949–0.979 | < 0.001 |
| c | 0.996 | 0.992–0.998 | < 0.001 |
Assessing the Weight-Bearing Line Ratio
The weight-bearing line (WBL) ratio is a critical parameter in evaluating knee joint alignment on radiographs. Determining it involves drawing a line from the center of the femoral head to the center of the ankle joint and assessing its intersection with the tibial plateau. The ideal WBL ratio indicates that the line passes through the medial tibial spine, which experts consider the mechanical axis of the lower limb.
When interpreting the WBL ratio, it is important to consider the patient’s overall limb alignment. A deviation from the ideal ratio may suggest underlying pathologies or the need for corrective measures. The following table presents a summary of WBL ratio values and their corresponding interpretations:
| WBL Ratio (%) | Interpretation |
| <20% | Lateral deviation |
| 20-40% | Normal alignment |
| >40% | Medial deviation |
The assessment of the WBL ratio is essential for diagnosing conditions such as osteoarthritis and planning surgical interventions like osteotomies. Accurate measurement of the WBL ratio can guide the treatment strategy and help predict postoperative outcomes.
Evaluating the Medial Proximal Tibial Angle
The Medial Proximal Tibial Angle (MPTA) is a critical parameter in assessing knee alignment and joint integrity. It is defined as the angle between the tibial mechanical axis and the line tangent to the articular surface of the proximal tibia. Accurate measurement of the MPTA is essential for diagnosing conditions such as varus or valgus deformities and planning corrective surgeries.
The MPTA reflects the knee’s structural alignment and is crucial for the joint’s biomechanics.
To ensure precision, the MPTA should be measured in a standardized manner, considering the medial edge of the proximal tibia and the point where the weight-bearing line intersects the articular surface. This measurement is crucial for evaluating the knee’s load-bearing capacity and for predicting the progression of degenerative diseases like osteoarthritis.
Here is a summary of the reliability of MPTA measurements from recent studies:
| Study | MPTA Reliability (95% CI) | P-value |
| A | 0.879 (0.814–0.921) | < 0.001 |
| B | 0.867 (0.727–0.935) | < 0.001 |
These values suggest a high level of consistency in MPTA assessment, which is vital for both clinical evaluations and research purposes.
Determining the Lateral Distal Femoral Angle
The lateral distal femoral angle (LDFA) is a critical parameter in assessing knee alignment. It is the angle between the femoral mechanical axis and the line tangent to the distal femur’s articular surface. Accurate measurement of the LDFA is essential for diagnosing and planning treatment for various knee conditions.
The LDFA provides insight into the distal femur’s alignment, which is crucial for maintaining proper knee joint mechanics.
Statistical analysis of radiographic measurements has shown high inter-observer reliability for the LDFA, indicating its importance and consistency in clinical assessments. The following table summarizes the reliability coefficients for the LDFA across different studies:
| Study | Inter-observer Reliability Coefficient | P-Value | |
| A | 0.927 – 0.985 | < 0.001 | |
| B | 0.940 – 0.988 | < 0.001 | |
| C | 0.961 – 0.988 | < 0.001 |
Measuring the Joint-Line Convergence Angle
The Joint line convergence angle (JLCA) is a critical parameter in assessing the congruity of the knee joint. It is defined as the angle is formed between a line tangential that touches the distal femoral condyle a line along the proximal tibia. Accurate measurement of the JLCA is essential for diagnosing conditions such as osteoarthritis and for preoperative planning.
The JLCA provides insight into the alignment and stability of the knee joint, which are vital for maintaining proper knee function.
To ensure precision, the JLCA should be measured under standardized conditions. Variability in this measurement can indicate changes in the joint space, which may be due to degenerative processes or other pathologies. The following table summarizes the average JLCA values obtained from a study, along with the standard deviation, indicating the variability among subjects:
| Measurement | Average JLCA (°) | Standard Deviation (°) |
| 1 | 1.88 | 2.25 |
| 2 | 1.88 | 2.25 |
These values provide a baseline for comparison when evaluating individual knee X-rays.
Interpreting the Posterior Tibial Slope
The posterior tibial slope (PTS) is a critical factor in knee radiograph interpretation, indicating the posterior inclination of the tibial articular surface. This slope can vary significantly between individuals, which may affect the measurement reliability of radiographic parameters. The PTS is particularly important when evaluating the joint line in anteroposterior (AP) images, as it reflects the morphology of the proximal tibial surface.
Variability in PTS can lead to differences in how the joint line appears on X-rays. For instance, a low PTS might show a distinct joint line, whereas a high PTS could result in an indistinct joint line. This variability is not only noticeable between the lateral compartments of the knee and medial but also among different individuals.
Understanding the PTS is essential for accurate assessment of knee radiographs, as it directly impacts the visibility and interpretation of the joint line and other key structures.
It is important for clinicians to recognize the influence of PTS on radiographic outcomes to ensure precise evaluation and diagnosis. The table below illustrates how the PTS can vary and its potential impact on radiographic clarity:
| PTS Degree | Joint Line Clarity |
| Low (2.2°) | Distinct |
| High (8.2°) | Indistinct |
Challenges in Knee Joint X-Ray Interpretation
Impact of Knee Flexion Angle on X-Ray Results
The knee flexion angle at the time of imaging significantly affects the accuracy of knee joint X-ray interpretation. Variations in flexion can obscure or distort key anatomical landmarks, leading to potential misdiagnosis or incorrect measurements of angles and distances.
The knee flexion angle is a critical factor that can alter the visibility of the articular surface and other important structures within the knee joint on an X-ray.
To ensure consistency and minimize errors, healthcare professionals often implement strict protocols during X-ray acquisition. These protocols aim to standardize patient positioning and the angle of the X-ray beam. Despite these efforts, some degree of variability is inevitable due to individual patient anatomy and movement.
Here is a summary of how knee flexion angles can impact specific radiographic parameters:
- Hip-knee-ankle angle: Can be overestimated or underestimated depending on the degree of flexion.
- Weight-bearing line ratio: May shift inappropriately, affecting the assessment of knee alignment.
- Medial proximal tibial angle: Susceptible to changes, influencing the perceived shape and orientation of the tibia.
- Lateral distal femoral angle: Can vary, altering the apparent angle between the femur and the knee joint.
- Joint-line convergence angle: Affected by knee position, potentially leading to incorrect conclusions about joint congruence.
Difficulties in Identifying Articular Surface Landmarks
The precision of radiographic measurements in knee evaluations is highly dependent on the clear identification of articular surface landmarks. In some cases, knee joint lines appear flattened or indistinct, making it challenging to determine the articular surface with accuracy. This difficulty can significantly affect the precision of measurements that rely on these reference points.
The X-ray beam angle during image acquisition and the positioning of the knee primarily influence the morphology of the tibial articular surface observed on the AP image.
Variability in the morphology of the proximal tibial surface, which differs between the medial and lateral aspects, adds to the complexity. Several factors, including the angle of the X-ray beam and the patient’s positioning during imaging, can influence the clarity of the joint line, which is crucial for accurate measurement. Additionally, the presence of effusion or synovial thickening can obscure joint lines, further complicating the identification process.
Recent advancements in technology suggest the potential for deep learning to aid in the detection of knee landmarks. This approach could automate the measurement of patellofemoral instability indices, which are related to patellar height and other critical dimensions, potentially improving the accuracy and consistency of radiographic evaluations.
Variability in Proximal Tibial Surface Morphology
The morphology of the proximal tibial surface is a critical factor in knee joint radiographic analysis. Variability in this area can significantly impact the accuracy of radiographic measurements, particularly those involving the joint line. The proximal tibial surface exhibits differences between the medial and lateral compartments, with notable inter-individual variations.
The posterior tibial slope (PTS) is a key aspect of the proximal tibial surface morphology. Anticipate that its variability among individuals will influence the measurement outcomes of radiographic variables.
In clinical practice, this variability may lead to inconsistencies in the appearance of knee joint lines on plain radiographs. Some may appear flattened, while others may be indistinct, complicating the assessment process. The significant inter-individual variability affects the PTS, which reflects the inclination of the tibial articular surface. This variability not only impacts joint biomechanics but also the measurement accuracy of related radiographic parameters.
Influence of Patient Positioning on Radiographic Accuracy
The precision of radiographic measurements is paramount in the diagnosis and management of knee conditions. Even slight deviations in patient positioning can lead to significant inaccuracies in interpreting radiographic data. For instance, the position of the patella, which is a critical landmark in knee radiographs, can be misrepresented if the patient’s leg is not correctly aligned.
- Proper alignment of the patient’s leg is essential.
- The X-ray beam angle must be consistent.
- To reduce variability, we should minimize the knee flexion angle.
Ensuring that the patient’s knee is in the correct position is not just about obtaining a clear image; it’s about capturing an accurate representation of the knee’s structure.
The impact of patient positioning is evident in the assessment of the posterior tibial slope (PTS), which can alter the appearance of the knee joint line and other parameters. A study has shown that higher PTS can decrease the reliability of measurements such as the Medial Proximal Tibial Angle (MPTA) and the Joint-Line Convergence Angle (JLCA).
Grading Osteoarthritis in Knee Radiograph
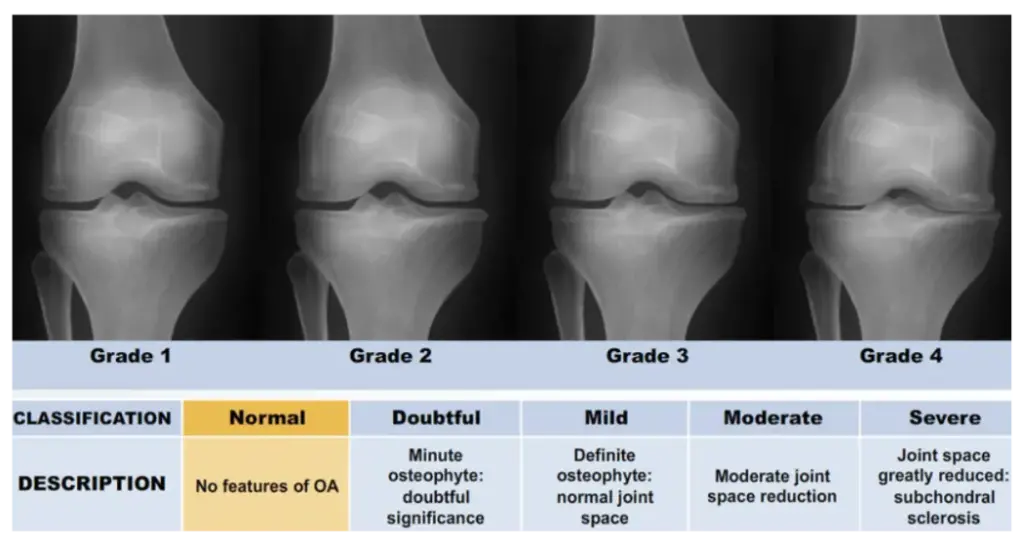
Utilizing the Kellgren-Lawrence Grading System
The Kellgren-Lawrence (K-L) grading system is a cornerstone in the radiographic assessment of osteoarthritis in knee joints. It provides a standardized approach to grading the severity of joint degeneration. This system is crucial for consistent communication among healthcare professionals and for monitoring disease progression. The K-L grades range from 0 to 4, with each grade reflecting the increasing severity of
osteoarthritis. Here is a brief overview of the grading scale:
- Grade 0: No radiographic features of osteoarthritis
- Grade 1: Doubtful joint space narrowing and possible osteophytic lipping
- Grade 2: Definite osteophytes and possible joint space narrowing
- Grade 3: Moderate presence of multiple osteophytes, clear narrowing of the joint space, some sclerosis, and potential bone contour deformity.
- Grade 4: Large osteophytes, significant narrowing of the joint space, extensive sclerosis, and definite deformity of bone contour.
Assessing the K-L grading system involves both fixed flexion weight-bearing anteroposterior (FLWAP) and knee posteroanterior (PA) radiographs, ensuring a comprehensive evaluation of the knee joint from different angles.
It is important to note that while the K-L grading system is widely used, it is not without limitations. The subjective nature of the grading can lead to variability between observers, which underscores the need for experienced radiologists and potentially supplementary imaging techniques.
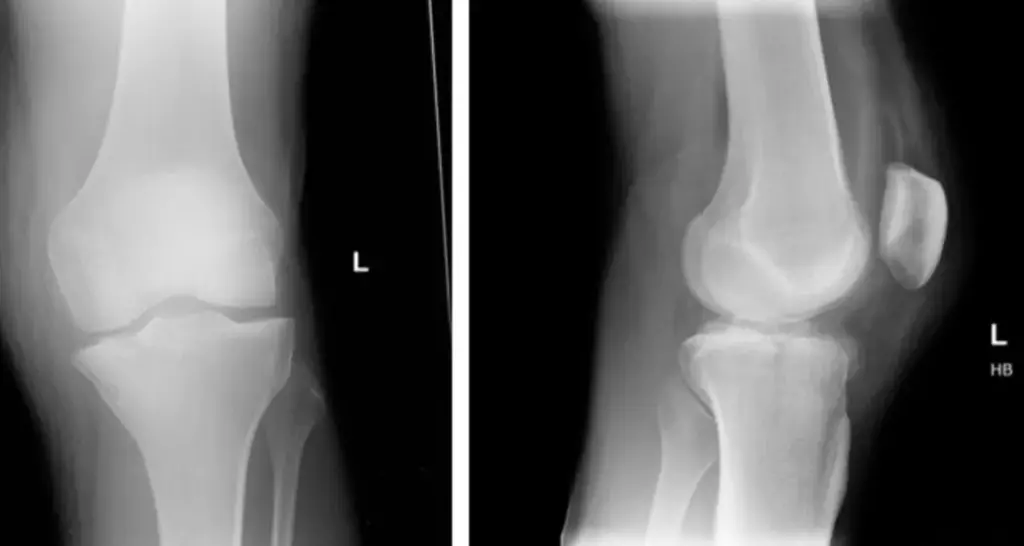
Comparing FLWAP and PA Radiograph Results
When comparing full-length weight-bearing anteroposterior (FLWAP) and posteroanterior (PA) radiographs, it’s crucial to understand the differences in their acquisition. FLWAP radiographs are taken with the patella facing the X-ray source, ensuring a consistent focus-to-film distance, which allows for a composite image to be formed. In contrast, PA radiographs are captured at approximately 30 degrees of knee flexion, providing a different perspective known as the schuss view.
The assessment of osteoarthritis using the Kellgren-Lawrence grading system is performed on both FLWAP and PA radiographs. Parameters such as the Hip-Knee-Ankle (HKA) angle, Weight-Bearing Line Ratio (WBLR), Medial Proximal Tibial Angle (MPTA), Lateral Distal Femoral Angle (LDFA), and Joint-Line Convergence Angle (JLCA) are measured primarily using FLWAP images.
It is important to note that patients unable to bear weight due to pain or discomfort are often excluded from FLWAP and PA radiographic analysis, which can impact the study’s demographic representation.
The following table summarizes the key differences in the acquisition of FLWAP and PA radiographs:
| Radiograph Type | Patient Positioning | Knee Flexion Angle | Image Composition |
| FLWAP | Patella facing X-ray source | None | Composite image |
| PA | Approx. 30° flexion | 30° (Schuss view) | Single image |
Correlating Osteoarthritis Grade with Radiographic Parameters
The correlation between osteoarthritis (OA) grade and various radiographic parameters is pivotal in understanding the progression of knee joint degeneration. These parameters include the hip-knee-ankle (HKA) angle, weight-bearing line ratio (WBLR), medial proximal tibial angle (MPTA), lateral distal femoral angle (LDFA), joint-line convergence angle (JLCA), and posterior tibial slope (PTS).
The Kellgren-Lawrence (K-L) grading system is commonly used to assess the severity of OA in both full-length weight-bearing anteroposterior (FLWAP) and posteroanterior (PA) knee radiographs. This grading is then mapped against the radiographic measurements to evaluate the structural changes in the knee joint.
Statistical analysis of these correlations can reveal significant patterns. For instance, a higher K-L grade often corresponds with increased deviations in angles such as the HKA and MPTA, suggesting a more advanced stage of OA. Below is a table summarizing the correlation coefficients between K-L grades and radiographic parameters from a sample study:
| Parameter | Correlation Coefficient (K-L Grade) |
| HKA Angle | 0.967 |
| WBLR | 0.990 |
| MPTA | 0.796 |
| LDFA | 0.951 |
| JLCA | 0.859 |
| PTS | Data not provided |
Statistical Analysis of Radiographic Measurements
Inter-observer Reliability in Parameter Assessment
The assessment of radiographic parameters can vary significantly between observers, which is a critical factor in ensuring the accuracy and reliability of knee X-ray interpretations. Inter-observer reliability is quantified using Intraclass Correlation Coefficients (ICCs), which measure the degree of agreement among different observers. For instance, the ICCs for the Medial Proximal Tibial Angle (MPTA) and the Joint-Line Convergence Angle (JLCA) tend to decrease as the Posterior Tibial Slope (PTS) increases.
The consistency of measurements between observers is paramount, as discrepancies can lead to divergent diagnostic conclusions and treatment plans.
The following table summarizes the ICC values for MPTA and JLCA across three different groups, illustrating the variability in measurement reliability:
| Group | MPTA ICC | JLCA ICC |
| A | 0.889 | 0.916 |
| B | 0.796 | 0.859 |
| C | 0.790 | 0.843 |
Significance of Radiographic Measurements Across Patient Groups
Radiographic measurements are pivotal in tailoring knee-related treatments to individual patient needs. Variability in these measurements can lead to different therapeutic approaches, affecting outcomes across diverse patient groups. For instance, in knee arthroplasty, precise radiographic data is crucial for implant positioning and alignment, which are directly linked to the success of the surgery.
The significance of radiographic measurements is further underscored when considering the management of knee disorders. These measurements guide the evaluation of disease progression and the effectiveness of interventions. In clinical settings, the following table illustrates the impact of radiographic measurements on patient management:
| Patient Group | Measurement Impact |
| Osteoarthritis | Treatment strategy adjustment |
| Ligament Injuries | Surgical planning refinement |
| Meniscus Tears | Postoperative management |
Ensuring consistency and reliability in these measurements is therefore a critical aspect of patient care, influencing both preoperative planning and postoperative assessment.
Evaluating the Consistency of Radiographic Parameter Measurements
The precision of radiographic measurements is crucial for accurate diagnosis and treatment planning. However, factors such as the Posterior Tibial Slope (PTS) can significantly affect the consistency of these measurements. Studies have shown that higher PTS values can lead to decreased reliability, particularly when assessing the knee joint line and angles like the Medial Proximal Tibial Angle (MPTA) and the Joint-Line Convergence Angle (JLCA).
The challenge of achieving consistent accuracy across different equipment and protocols is compounded by the complex morphology of the knee joint. Variability in the proximal tibial surface morphology, for instance, can introduce discrepancies in measurements.
To better understand the impact of PTS on measurement reliability, researchers have categorized patients into groups based on their PTS values. This stratification allows for a more nuanced analysis of how slope variations influence measurement consistency. While efforts are made to control confounding factors, it is acknowledged that not all variables affecting measurement reliability can be fully managed.
Clinical Relevance of Radiographic Findings
Implications for Surgical Planning and Treatment
Radiographic evaluations of the knee joint are pivotal in surgical planning.
Precise preoperative measurements are essential for guiding procedures like high tibial osteotomy and total knee arthroplasty, directly influencing surgical outcomes. Postoperative radiographs are equally critical, informing the ongoing management of patients. Radiographic assessments, particularly in the coronal plane, are integral to clinical practice, influencing decisions in cases of osteoarthritis, fractures, and ligament injuries.
Minor inaccuracies in radiographic measurements can lead to significant clinical consequences. Treatment strategies hinge on these assessments, necessitating precision and care in their interpretation. For instance, the medial proximal tibial angle (MPTA) and joint-line convergence angle (JLCA) must be evaluated with consideration for the posterior tibial slope (PTS), as a high PTS can affect the reliability of these measurements.
- Preoperative Assessment: Ensures correct surgical intervention.
- Postoperative Assessment: Guides patient recovery and future care.
- Coronal Plane Radiographs: Most commonly used in clinical evaluations.
- Measurement Accuracy: Critical for successful clinical outcomes.
Understanding the Relationship Between Radiographic Parameters and Knee Function
The intricate relationship between radiographic parameters and knee function is pivotal in the clinical management of knee disorders. Radiographic parameters such as the hip-knee-ankle (HKA) angle, weight-bearing line ratio (WBLR), and medial proximal tibial angle (MPTA) are not just mere measurements; they are critical indicators that guide treatment strategies and surgical planning.
An accurate assessment of these parameters is essential for predicting surgical outcomes and ensuring successful rehabilitation.
For instance, a high posterior tibial slope (PTS) has been linked to increased risks in knee-related conditions. A study highlighted the importance of radiomics analysis of the patellofemoral joint for improved knee risk prediction. The following table summarizes the key radiographic parameters and their relevance to knee function:
| Parameter | Relevance to Knee Function |
| HKA Angle | Alignment and stability |
| WBLR | Load distribution |
| MPTA | Joint congruence |
| LDFA | Femoral orientation |
| PTS | Slope and biomechanics |
Using Radiographic Data to Predict Disease Progression
Radiographic data plays a pivotal role in predicting the progression of knee osteoarthritis and other degenerative conditions. Accurate radiographic measurements are crucial for forecasting the course of the disease and tailoring patient-specific management plans. For instance, the alignment of the knee joint as seen on X-rays can indicate the likelihood of disease progression and the potential need for intervention.
- Alignment: Deviations in knee alignment can suggest an increased risk of osteoarthritis progression.
- Joint space narrowing: This is a direct indicator of cartilage loss and can signal advancing disease.
- Osteophyte formation: The presence of bone spurs is associated with disease severity and can predict further joint degeneration.
The integration of clinical features with radiographic assessments, such as the ACR criteria, enhances the predictive accuracy for disease progression.
The use of advanced imaging techniques and analytical tools, including deep learning algorithms, has shown promise in improving the predictive power of radiographic data. These innovations may soon allow for more precise predictions based solely on knee anteroposterior radiographs, potentially reducing the need for more extensive imaging.
Conclusion
In conclusion, understanding a knee joint X-ray involves recognizing normal anatomical structures and variations, as well as accurately interpreting radiographic parameters. Despite the challenges posed by individual morphological differences and technical aspects of image acquisition, this article has outlined the key factors that contribute to a normal knee X-ray result. By adhering to strictly controlled conditions and excluding images potentially affected by knee flexion or patient position, we can minimize bias and enhance the precision of measurements.
The radiographic parameters discussed, such as the hip-knee-ankle angle, weight-bearing line ratio, and joint-line convergence angle, are essential in assessing the knee’s condition. It is important for practitioners to be aware of the potential for variability and to apply consistent standards when evaluating knee radiographs to ensure accurate diagnosis and treatment planning.
Frequently Asked Questions
What are the key radiographic parameters for evaluating a knee joint X-ray?
Key parameters include the hip-knee-ankle (HKA) angle, weight-bearing line ratio (WBLR), medial proximal tibial angle (MPTA), lateral distal femoral angle (LDFA), joint-line convergence angle (JLCA), and posterior tibial slope (PTS).
How does knee flexion angle impact X-ray results?
Knee flexion angle can affect the appearance of the articular surface on X-rays. Strictly controlled anterior-posterior radiographs are used to minimize bias from knee flexion or patient position.
What is the Kellgren-Lawrence grading system used for?
The Kellgren-Lawrence grading system is used to assess the severity of osteoarthritis in knee radiographs, ranging from grade 0 (no osteoarthritis) to grade 4 (severe osteoarthritis).
Why is it challenging to identify articular surface landmarks on knee X-rays?
The precision of identifying articular surface landmarks can be compromised due to factors like the X-ray beam angle, knee positioning, and individual morphological variability of the knee joint.
How is the consistency of radiographic measurements evaluated?
Consistency is evaluated through statistical analysis such as inter-observer reliability assessments and comparing measurements across different patient groups.
What is the clinical relevance of radiographic findings in knee X-rays?
Radiographic findings are crucial for surgical planning and treatment, understanding the relationship between radiographic parameters and knee function, and predicting disease progression.
If you are looking for a second opinion on your X-ray or if you have questions about your X-ray. Feel free to schedule a consultation with our office, we specialize in natural pain management and regenerative medicine. You can reach us by contacting us at 727-550-0855, or you can click the link below to schedule a consultation with us.


