X-ray imaging is a crucial diagnostic tool in orthopedics, particularly for assessing the complex structure of the knee joint. This article explores the anatomy of a healthy knee joint as seen in X-rays. It examines various radiographic techniques and their clinical relevance. We also compare advanced imaging methods like MRI and CT scanning, and their roles in diagnosing knee conditions. Finally, we explore imaging-based functional assessment of the knee joint and discuss when to indicate certain diagnostic procedures.
Key Takeaways
- X-ray imaging efficiently identifies bone fractures and assesses knee joint anatomy. Axial and lateral views offer varied perspectives for optimal visualization.
- The axial view radiograph is most accurate when the knee is at 20-45 degrees of flexion. The lateral view has shown high sensitivity in detecting fractures.
- MRI provides detailed imaging of soft tissues without radiation exposure. CT scans offer more precise measurements, like the TT-TG distance for preoperative planning.
- Ultrasound imaging is beneficial for evaluating soft tissue structures such as bursae. MRI is particularly useful for diagnosing arthritis and assessing patellofemoral dynamics.
- Functional assessments of the knee joint, such as evaluating patellar biomechanics and the Q angle. These are essential in diagnosing conditions like patellar instability and planning treatment.
Understanding Knee Joint Anatomy Through X-Ray Imaging

Components of a Healthy Knee Joint
The knee is the largest joint in the body, functioning as a hinge to connect the femur, tibia, and patella. Two types of cartilage support this complex structure: the meniscus, which absorbs shock, and the articular cartilage, providing a smooth, gliding surface for joint movement.
Synovial fluid within the knee joint serves as a lubricant, reducing friction and allowing for seamless motion. This fluid, along with the cartilage, is crucial for the knee’s ability to bear weight during activities such as walking and climbing stairs.
Four main ligaments contribute to the knee’s stability: the ligament (ACL), anterior cruciate , medial collateral ligament (MCL), posterior cruciate ligament (PCL), and lateral collateral ligament (LCL) collaborate harmoniously to uphold correct alignment and deter undue movement that may result in injury.
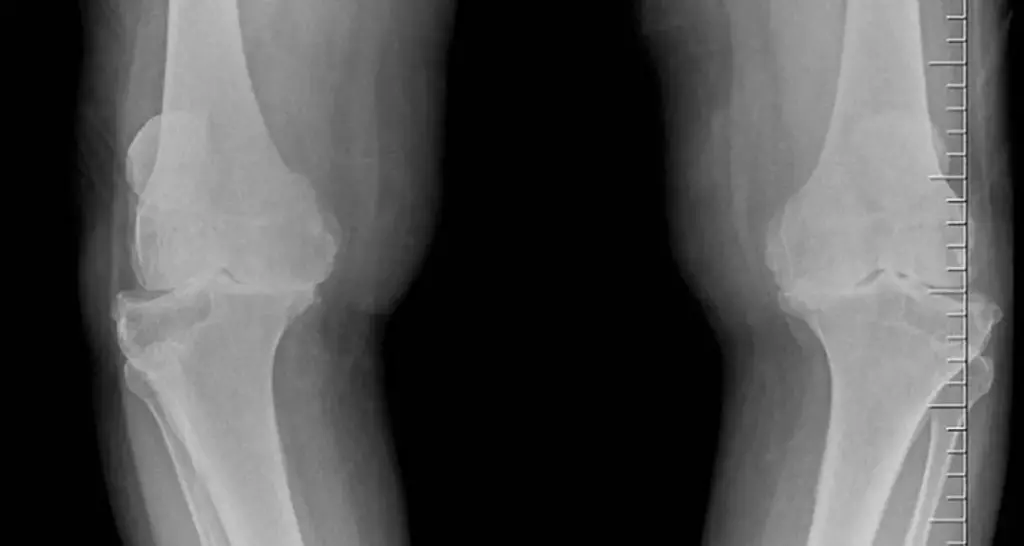
Identifying Key Structures in X-Ray Images
When reviewing knee radiographs, it’s essential to have a systematic approach to ensure all key structures are identified and assessed. It effectively communicates the idea that the ability to distinguish between normal and abnormal findings is essential for accurate diagnosis and treatment planning. A typical X-ray of the knee joint will display various bones such as the femur, tibia, and patella, as well as joint spaces and surrounding soft tissues.
In a healthy knee X-ray, the joint space should appear even and clear, indicating well-preserved cartilage. Any deviations from this norm may suggest underlying issues such as arthritis or injury.
Understanding the nuances of knee X-ray interpretation requires familiarity with the anatomy and the common radiographic views used. For instance, the axial view is particularly helpful for examining the patellofemoral joint, while the lateral view is sensitive in detecting fractures. Here’s a simple list to guide the identification process:
- Femur: The thigh bone, largest in the knee joint
- Tibia: The shin bone, key to weight-bearing
- Patella: The kneecap, aids in knee extension
- Joint space: Indicates cartilage health
- Soft tissues: Includes muscles and ligaments
Comparing X-Ray Views for Optimal Visualization
To fully appreciate the intricacies of the knee joint, it is essential to compare different X-ray views. Each view can reveal distinct aspects of the knee’s anatomy, providing a comprehensive understanding of its structure. For instance, the axial view radiograph, commonly taken with the patient supine position and the knee flexed at 20-45 degrees, can be particularly telling of the patella position and the trochlear groove alignment.
The lateral view is invaluable for fracture detection. A study showed a single lateral view radiograph had 100% sensitivity in identifying fractures. This underscores its importance in acute trauma cases.
While plain radiography excels in revealing bone structures and fractures, it falls short in soft tissue assessment. Here, MRI and ultrasound imaging take precedence, offering detailed images of soft tissues such as bursae without the use of radiation. The selection of an imaging technique depends on the clinical scenario and the specific details needed for diagnosis or treatment planning.
Radiographic Techniques and Their Clinical Relevance
Axial View Radiography and Flexion Angles
Axial view radiography is a pivotal technique in assessing knee joint health, particularly for detecting fractures and evaluating patellar alignment. The optimal flexion angle for axial views ranges from 20 to 45 degrees. This allows for a clear depiction of the patella in relation to the femur and tibia. This range of flexion is crucial as it provides the best compromise between image clarity and patient comfort.
Combining the axial view with external rotation of the tibia can notably enhance visualization of specific knee structures. In clinical practice, comparing the axial view with other imaging modalities ensures a comprehensive assessment. For instance, MRI offers no radiation exposure, while CT scans provide finer detail with smaller cuts. This is crucial for precise measurements, such as the trochlea-tubercle distance.
When interpreting axial radiographs, one must consider the patient’s specific anatomy and any potential laterally directed vectors on the patella. A structured approach to analyzing these images can greatly assist in diagnosing and managing patellofemoral dysfunction.
Sensitivity of Lateral View Radiographs in Fracture Detection
The lateral view radiograph is a critical tool in the detection of knee fractures. A study involving 214 patients with acute knee trauma revealed a 100% sensitivity for detecting fractures using a single lateral view radiograph. This high level of accuracy underscores the importance of this imaging technique in the initial assessment of knee injuries.
The lateral view not only identifies patellar, tibial, and femoral fractures but also reveals patellar height and tilt. Additionally, it shows trochlear depth, crucial for diagnosing patellofemoral pain and subluxation.
While the lateral view radiograph excels in fracture detection, it has limitations in evaluating soft-tissue structures. For a more comprehensive assessment, other imaging modalities such as CT scanning or MRI may be required. The table below summarizes the sensitivity of different radiographic views in detecting knee fractures:
| Radiographic View | Sensitivity (%) |
| Lateral View | 100 |
| Axial View | Data Not Provided |
| Other Views | Data Not Provided |
It’s evident that the lateral view radiograph is crucial in the diagnostic process, especially when fractures are suspected. Clinicians must, however, be aware of its limitations and consider additional imaging techniques for a complete evaluation.
Dynamic CT Scanning for Patellofemoral Dynamics
Dynamic CT scanning offers a more nuanced view of the patellofemoral joint by capturing its motion in real-time. This technique excels at assessing in vivo physiological relationships. It involves a helical CT scanning process with continuous 10-second exposure at the midtrochlea level.
CT scanning surpasses plain radiography in its ability to image patellar cartilage and calculate the TT-TG distance from axial scans, which is crucial for surgical planning.
Studies have demonstrated that CT scanning is approximately 1.5 times more sensitive than standard radiography in detecting patellar tracking anomalies.
It has proven highly effective in determining the severity of patellar tilt and subluxation. This aids in selecting appropriate surgical interventions, such as lateral retinacular release.
While MRI is more costly, it excels over CT in identifying patellar chondral lesions. It also measures cartilage thickness and volume, vital for diagnosing osteoarthritis and planning surgical outcomes. Despite its clinical value, kinematic MRI is not widely available and may not be necessary for most patients.
Advanced Imaging Modalities for Knee Assessment
MRI vs. CT Scanning: A Comparative Analysis
When assessing the health of a knee joint, both MRI and CT scans offer valuable insights, but they do so through different mechanisms. MRI is renowned for its superior ability to visualize soft tissues, such as cartilage. This makes it particularly effective for diagnosing conditions like osteoarthritis or patellar chondral lesions. MRI’s detailed images enable precise measurements of cartilage thickness and volume. These measurements are crucial for evaluating joint health and planning surgical interventions.
CT scans, on the other hand, have their own set of advantages. They are more sensitive than standard radiography in detecting conditions such as patellar subluxation. Additionally, they can perform dynamic studies assessing patellofemoral dynamics in vivo. Despite this, CT scans are less sensitive than MRIs for detecting lesions in cartilage and require the use of contrast media for certain studies. Additionally, CT scans expose patients to radiation, which is a notable disadvantage compared to MRI.
Both imaging modalities have clinical applications that make them indispensable in the field of orthopedics. The decision between MRI and CT scanning frequently hinges on the particular clinical scenario and the specific information sought by the physician.
Here is a comparative summary of MRI and CT scanning for knee assessment:
- MRI:
- Superior soft tissue visualization
- No radiation exposure
- More effective for cartilage assessment
- CT Scanning:
- More sensitive than radiography for patellar tracking anomalies
- Can perform dynamic studies
- Exposes patients to radiation
Understanding the limitations and strengths of each modality facilitates a more informed decision-making process when diagnosing and treating knee joint conditions.
Ultrasound Imaging for Soft Tissue Evaluation
Ultrasound imaging is a versatile tool in the evaluation of soft tissue structures within the knee joint. Unlike X-ray, which is adept at visualizing bone, ultrasound excels in distinguishing between different types of soft tissues, such as ligaments, tendons, and bursae. This makes it particularly useful for diagnosing conditions that may not be evident on traditional radiographs.
Ultrasound can play a crucial role in identifying the cause of anterior knee pain. It offers a non-invasive method to differentiate between various pathologies such as cysts, granulation tissue, and mucinoid degeneration.
In knee bursitis, ultrasound imaging detects swelling in the affected bursa. This aids healthcare professionals in accurate diagnosis and management.The ability to visualize soft tissue in real time also allows for guided interventions, such as aspirations or injections, enhancing the precision of treatment.
The following list highlights the advantages of ultrasound imaging in knee assessment:
- Superior to CT in distinguishing soft tissue variations
- Real-time imaging capability for guided procedures
- Non-invasive and does not involve ionizing radiation
- This imaging modality can integrate with other techniques for a comprehensive evaluation
The Role of MRI in Diagnosing Arthritis
Magnetic Resonance Imaging (MRI) stands as a powerful tool for both early detection and effective management of arthritis. It provides detailed images of joints, bones, and surrounding soft tissues, highlighting the presence of inflammation, cartilage damage, and other signs indicative of arthritis. This level of detail assists clinicians in formulating a precise diagnosis and tailoring treatment plans effectively.
- MRI scans can reveal early signs of arthritis, often before symptoms become severe.
- They are particularly adept at showing soft tissue changes, including swelling and inflammation.
- MRI can also identify bone spurs or cysts, as well as cartilage or bone fragments within the joint fluid.
MRI’s ability to visualize the intricate structures of the knee joint makes it an indispensable modality in the diagnosis and ongoing assessment of arthritis. Its sensitivity to changes in soft tissue and bone composition provides a comprehensive view that is not possible with X-rays alone.
The use of MRI in diagnosing arthritis is not only about detecting the condition but also about monitoring its progression. By comparing sequential MRI scans, doctors can evaluate the efficacy of treatment and make necessary adjustments to optimize patient outcomes.
Functional Assessment of the Knee Joint
Evaluating Patellar Biomechanics and Stability
The patellar tendon, which is essential for the knee joint, plays a crucial role in stability maintenance and facilitating movement. Its biomechanical and viscoelastic properties can be quantitatively evaluated to assess the health of the knee joint. Elastography, a technique that measures the stiffness of soft tissues, has emerged as a valuable tool in this context.
Factors contributing to patellar stability include the morphology of the patellar insertion, the strength and timing of the vastus medialis muscle, and the alignment of the patella within the intercondylar notch. These factors can be influenced by both anatomical variations and the presence of orthotic devices.
The evaluation of patellar biomechanics is not only about understanding the forces at play but also about recognizing the intricate balance that ensures knee stability and function.
Surgical interventions, such as lateral retinacular release, are sometimes necessary to correct patellar instability. However, the decision to operate should be made cautiously, considering the potential effects on the lateral stability of the patella.
Assessing Trochlear Depth and Patella Position
The assessment of the trochlear depth and patella position is a critical aspect of diagnosing patellofemoral disorders. A true lateral view is often utilized to evaluate these features, providing insights into conditions such as patella alta or baja, and patella tilt. This perspective is particularly sensitive for detecting patellofemoral pain and previous subluxation.
In the lateral view, the proximal portion of the trochlear groove can be examined for signs of dysplasia, which is essential for understanding patella motion in early flexion. Notably, trochlear dysplasia is a morphological deformity associated with patellofemoral instability.
To quantify the trochlear depth, radiologists may look for specific signs on lateral radiographs, such as the supratrochlear spur, crossing sign, and double contour sign. These are part of the Dejour classification, which helps in identifying the severity of trochlear dysplasia. Additionally, axial views on MRI or CT scans can be used to measure the trochlea-tubercle distance, which reflects the lateral forces acting on the patella. A distance of 2 cm is considered specific for lateral vector assessment, though not highly sensitive.
The Importance of the Q Angle in Knee Function
The Q-angle, or quadriceps angle, is a critical measurement for assessing the alignment of the knee joint. It is defined as the angle formed by the quadriceps tendon and the patellar tendon. A normal Q-angle ensures that the patella tracks properly within the trochlear groove during knee flexion and extension movements.
An abnormal Q-angle may signal potential knee issues, such as patellofemoral pain syndrome or patellar instability. It is important for clinicians to measure this angle accurately, as it can influence the approach to treatment and rehabilitation. The Q-angle can be measured in various positions, but commonly while the patient is standing or with the knee at 20° of flexion.
The Q-angle provides useful information about the knee joint’s alignment and is a significant factor in the biomechanics of the knee. An increased Q-angle is often associated with a higher risk of knee injuries and can guide the need for corrective procedures.
Clinicians should be mindful of the typical ranges of the Q-angle, which may exhibit slight variations between men and women. Regular assessment of the Q-angle is essential in the functional evaluation of the knee, especially in athletes and individuals with knee pathologies.
Diagnostic Procedures and Their Indications
When to Consider Knee Aspiration
Knee aspiration, also known as arthrocentesis, is a procedure where fluid is drained from the knee joint. This is often performed when there is an accumulation of excess fluid, such as in cases of knee effusion, to relieve pain, reduce swelling, and improve joint function. The procedure can also be diagnostic, helping to determine the cause of joint swelling by analyzing the aspirated fluid. However is this is being done for pain management, it should be done as a last resort, since often times aspiration will give relief in the short term, but often times in the long run there is a chance of excess fluid accumulation.
Indications for knee aspiration include:
- Knee effusion of unclear etiology
- Evaluation for septic knee
- Suspected gouty arthritis
- Knee osteoarthritis requiring therapeutic injection
Aspiration might cause mild short-term pain, but it is generally a safe procedure. After aspiration, some patients may need to immobilize the knee to aid in healing and prevent recurrent effusion.
While knee aspiration can be therapeutic, it is also a valuable diagnostic tool. In cases where infection or gout is suspected, analyzing the aspirated fluid can provide crucial information for appropriate treatment.
Interpreting the Apprehension Sign
The apprehension sign is a clinical test utilized to evaluate the stability of the patellofemoral joint. When a patient exhibits a sense of apprehension or discomfort as the patella is gently pushed laterally, it suggests potential instability or previous dislocation. This test is particularly telling in a flexed knee position, where the patella is more likely to engage with the trochlea.
The apprehension sign indicates potential instability and also gauges the patient’s psychological response to patellar movement. This aspect can be crucial for designing rehabilitation strategies.
Understanding the nuances of this test can guide further diagnostic imaging. For instance, the height of the patella can be assessed with the knee in 30 degrees of flexion, either on lateral radiograph, sagittal computed tomography (CT), or magnetic resonance imaging (MRI). These imaging techniques can provide a clearer picture of the anatomical factors contributing to the instability.
Utilizing Imaging for Preoperative Planning
In the realm of orthopedic surgery, preoperative planning is crucial for successful outcomes, particularly in the context of knee surgeries. Imaging plays a pivotal role in this preparatory phase, offering a detailed blueprint of the knee’s anatomy and potential issues that may need to be addressed during the procedure.
Imaging modalities such as plain radiography, CT scanning, and MRI are commonly employed to assess the knee joint before surgery. Each modality provides unique insights:
- Plain radiography is cost-effective and widely used for initial screening, capturing anteroposterior, lateral, and axial views.
- CT scans offer detailed images of bone structures and are particularly useful for dynamic studies, evaluating patellofemoral dynamics, and measuring the TT-TG distance.
- MRI excels in depicting soft tissue details, aiding in the visualization of bursae, ligaments, and cartilage.
The integration of these imaging techniques into preoperative planning enhances the surgeon’s ability to anticipate challenges and tailor the surgical approach to the individual patient’s anatomy.
Choosing the correct imaging test is essential, depending on the particular clinical scenario. For instance, while an X-ray might suffice for detecting bone abnormalities or arthritis, an MRI would be the preferred choice for soft tissue evaluation. The ultimate goal is to utilize imaging to minimize intraoperative surprises and optimize patient outcomes.
Conclusion
In summary, the exploration of a healthy knee joint through various imaging techniques, including X-rays, MRI, and CT scans, provides a comprehensive understanding of its anatomy and function. While plain radiography is a cost-effective and efficient method for detecting bone fractures and assessing the knee’s structural integrity, its limitations in visualizing soft tissues are well-addressed by MRI and ultrasound.
The use of axial views, lateral views, and dynamic CT scanning offers detailed insights into the patellofemoral relationship, trochlear morphology, and the biomechanics of the knee. As we’ve seen, these imaging modalities are invaluable tools for diagnosing conditions, planning surgeries, and ensuring the maintenance of knee health. Ultimately, a normal X-ray of the knee joint is just the starting point for a deeper investigation into the complexities of this essential and intricate joint.
Frequently Asked Questions
What is the standard flexion angle for an axial view knee radiograph?
The standard flexion angle for an axial view knee radiograph is typically 20-45 degrees, with and/or without external rotation of the tibia.
How effective are lateral view radiographs in detecting knee fractures?
Lateral view radiographs are highly effective in detecting knee fractures, with a study showing 100% sensitivity in a sample of 214 patients with acute knee trauma.
What benefits does MRI offer compared to CT scanning for knee assessment?
MRI provides the advantage of radiation-free imaging and delivers detailed images of soft tissues, making it invaluable for assessing conditions while avoiding exposure to ionizing radiation.
When should knee aspiration be considered?
Knee aspiration should be considered when there is a need to relieve pain due to fluid accumulation, however this should be a last resort. Although a patient may experience relief after aspiration, there is a risk of that fluid returning and sometimes even returning with even more fluid accumulation. However it is vital if you are using aspiration as a diagnostic tool to analyze the fluid for infection, arthritis, or other conditions.
What does the apprehension sign indicate in knee examination?
The apprehension sign indicates potential medial instability of the knee when lateral pressure is applied at 30 degrees of flexion, causing apprehension or discomfort for the patient.
How does CT scanning contribute to preoperative planning for knee surgeries?
CT scanning can provide detailed images of patellar cartilage and calculate the TT-TG distance on axial scans, which is crucial for evaluating patellofemoral relationships and planning surgical interventions.
If you have any further questions about your knee X-rays, MRI’s or CT scans or if you would like to have a second opinion about your knee feel free to contact us at Waters Edge Medical Clinic and Spa our office is located at 1700 66th St. N. Suite 304, St. Petersburg, Fl. 33710. Our office phone number is 727-550-0855. Feel free to contact us, or use the scheduling link to set up a free consultation and evaluation.


